Overview
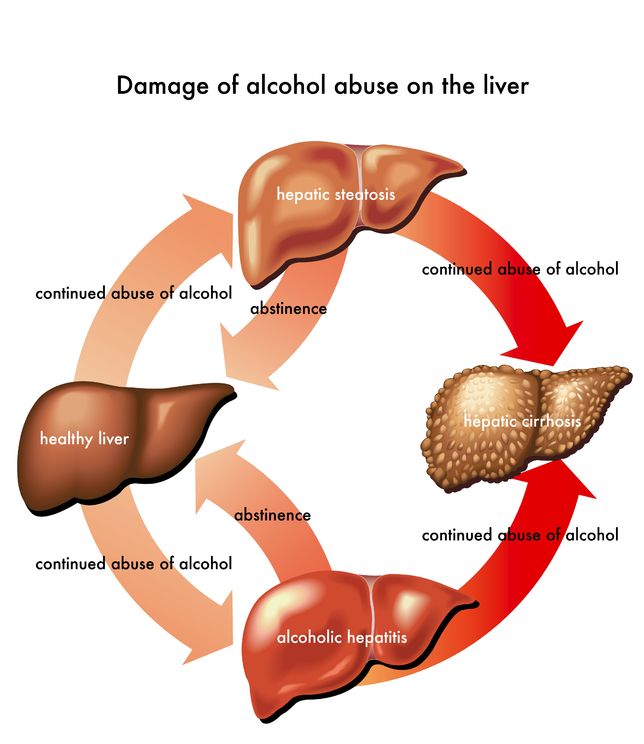
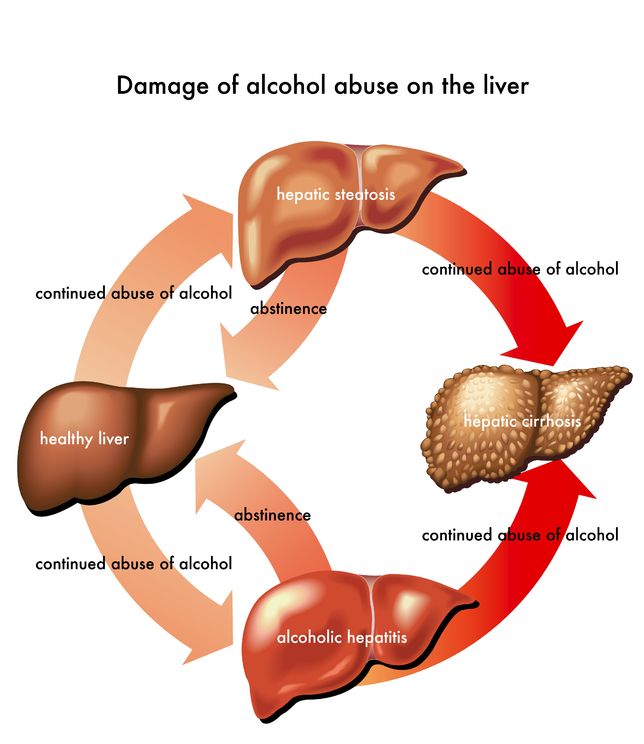
The term “alcoholic liver disease” refers to a set of progressive hepatic conditions that result from the long-term alcohol abuse. It comprises the following diseases: fatty liver, alcoholic hepatitis and cirrhosis.Fatty liver disease occurs after acute alcohol ingestion. If abstinence or moderate alcohol consumption is adopted, the situation is easily reversible and does not predispose to any serious, chronic liver diseases.
Alcoholic hepatitis tends to develop after a sustained consumption of a large amount of alcohol over time. The liver disorders that the patients may have can range from asymptomatic biochemical alterations to the fulminant liver failure.
Cirrhosis occurs later in the course of the disease and it is characterized by the replacement of the normal, functional tissue of the liver by fibrous tissue. Fibrous tissue does not perform normal hepatic functions, thus producing specific clinical manifestations. Liver cirrhosis is usually considered irreversible.
Alcoholic liver disease is accountable for many cases of mortality and morbidity worldwide.
Symptoms
Fatty liver disease is frequently asymptomatic or presents with nonspecific symptoms, which rarely suggest the presence of acute liver disease. Upon physical examination, the doctor may identify an enlarged, sometimes tender liver. If the accumulation of fat in the liver is stern, the patient may complain of weakness, abdominal pain, nausea, loss of appetite and a general feeling of discomfort.The spectrum of alcoholic hepatitis’ severity is rather extensive, meaning that the patients can present with a variety of manifestations. Less specific symptoms include abdominal pain and distension, nausea, vomiting, anorexia and weight loss. More serious symptoms can include liver failure and encephalopathy. Physically, the patient might have jaundice (yellowing of the skin and whites of the eyes), spider angiomas (spider-like veins on the skin) and enlargement of the liver.
Patients with alcoholic cirrhosis typically have the same symptoms as patients with cirrhosis with a different origin. These include jaundice, generalized itching, abnormal lab results, bleeding gums and/or nose and vomiting, among others.
Risk factors
The main factors recognized to increase the risk of alcoholic liver disease are:- Consumption of high quantities of alcohol, maintained over a prolonged period of time
- Being a female increases the susceptibility of having the disease
- A concomitant hepatitis C infection
- Certain genetic factors
- Malnutrition, especially vitamin A and E deficiencies. These deficiencies are very common in people who have drinking problems, because they often neglect their diets
- Hemochromatosis, a medical condition characterized by iron overload
Diagnosis
With the majority of patients having no symptoms, fatty liver disease is typically diagnosed after the identification of abnormal biochemical parameters. Some ultrasonographic findings are characteristic of fatty liver disease but do not allow for the identification of its cause (alcohol, insulin resistance, malnutrition, drug side effects, etc.). Consequently, to attribute a fatty liver disease to alcohol consumption, a detailed and accurate patient history must be obtained.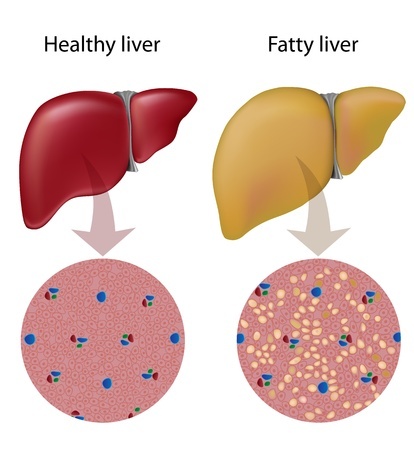
The diagnosis of alcoholic hepatitis also relies on a complete patient history, complemented with a physical examination and laboratory tests. The tests focus on the measurement of substances produced by the liver that can be found in the bloodstream. For a definite diagnosis, a liver biopsy might be necessary.
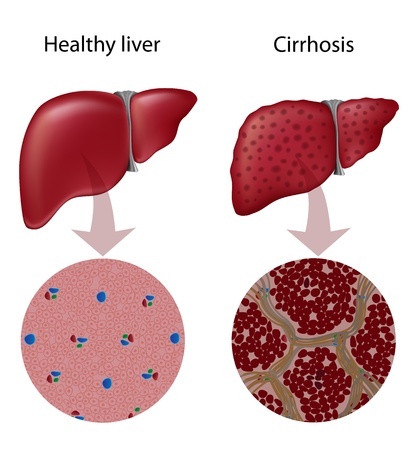
Diagnosing of alcoholic cirrhosis also depends on the combining physical and lab observations with a history of excessive alcohol intake over time. Most of the time, doctors can quickly associate the reported signs and symptoms and the liver biopsy findings with alcoholic cirrhosis and decide on the best course of treatment.
Treatment
The first step in the treatment of alcoholic liver disease is the ending of alcohol consumption. In some cases, the patient might need to be accompanied by a specialized team and, as such, the referral to an adequately qualified team is essential.- Nutritional supplementation - Because most patients with alcoholic liver disease have a tendency to neglect their diets, nutritional support must be provided for all patients. Adequate protein intake must be ensured. Nutritional supplementation may help improve the liver function.
- Drugs - Certain drugs can help patients deal with the liver damage and its associated symptoms. These include corticosteroids, colchicines, propylthiouracil, insulin, glucagon and others.
- Liver transplantation - Liver transplantation might be an option for patients with such a high degree of liver damage that no other approaches seem effective. However, liver donors are scarce in most countries and waiting lists tend to be long.