Overview
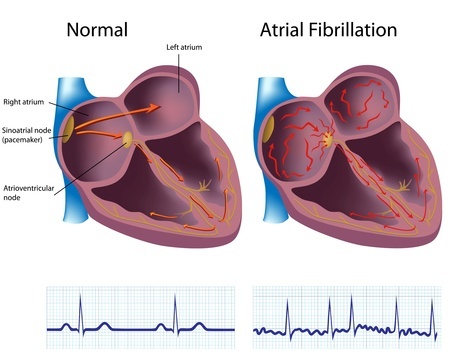
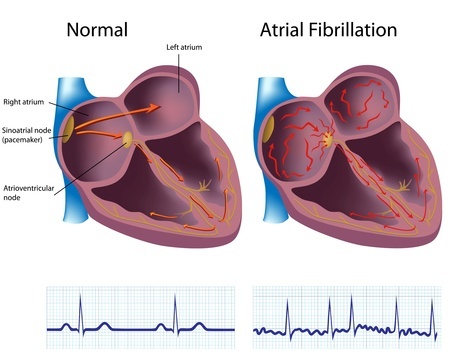
Atrial fibrillation or flutter (also referred to as AF or Afib) is the most common type of cardiac arrhythmia. This is a problem with the rate, or rhythm, of the heartbeat (heart rhythm disorder). It affects between 0.4 and 1% of all people, and its occurrence increases with the age.Each heartbeat involves contraction of two upper chambers of the heart (atria), followed by contraction of the two lower chambers (ventricles). The contractions are precisely guided by the electrical system of the heart which controls the rate and rhythm of the heartbeat. In normal heart, an electrical signal or impulse spreads from the top to the bottom of the heart in an orderly manner.
In case of Atrial fibrillation, the electrical impulses begin in a different part of the heart. The electrical signals do not spread normally throughout the atria. Instead, they travel in a rapid, disorganized manner, causing the atria to contract very fast and irregularly, or fibrillate. Overall, this results in an equally rapid and disorganized heartbeat pattern. This is accompanied by an inadequate filling and ejecting of blood from the heart chambers. This results in a poor blood flow to the body. Atrial fibrillation can produce a life threatening situation.
Symptoms
Atrial fibrillation may occur without any symptoms at all, and people with atrial fibrillation often live normal, active lives. Signs and symptoms of atrial fibrillation may include:
- Fatigue or lack of energy
- Dizziness (feeling faint or light-headed) or confusion
- Heart palpitations (a sudden pounding, fluttering, or racing feeling in the chest)
- Sensation of chest discomfort (pain, pressure, or tightness in the chest)
- Difficulty breathing during normal activities or even at rest (shortness of breath)
- Decreased blood pressure
- Weakness
Risk factors
Risk factors for atrial fibrillation include:- Age 60 and over
- Being white and male
- A family history of atrial fibrillation
- Metabolic conditions, such as hyperthyroidism or diabetes
- Long-term heavy alcohol use
- Certain metabolic conditions, such as hyperthyroidism or diabetes
- Obesity
- Obstructive sleep apnea
- Hypertension
- Heart failure
- Heart valve disease
- Heart surgery
- Coronary artery disease and heart attack
- Stimulants such as theophylline, amphetamines, pseudoephedrine, cocaine, methamphetamines, and excessive nicotine or caffeine.
Diagnosis
Atrial fibrillation (AF) is diagnosed primarily based on patient's medical and family history, physical examination and the results from diagnostic tests and procedures.Diagnostic tests and procedures include:
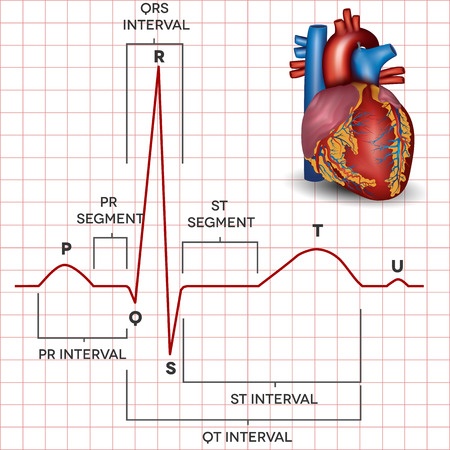
- Electrocardiogram (ECG) - a noninvasive test, for which electrodes are attached to the skin to measure the electrical impulses generated by the heart. Impulses are recorded as waves, displayed and analyzed.
- Holter monitor - a portable device which records the information about the electrical activity of the patient's heart for a day or two during normal activities. The patient can press a button if he/she feels symptoms, so the doctor can know what heart rhythm was present at that moment.
- Event recorder - a device similar to a Holter monitor with the exception that not all of the patient's heartbeats are recorded. The signals are recorded or transmitted from the device while patient is experiencing symptoms.
- Echocardiogram - a noninvasive test, in which sound waves are used to produce a video image of the patient's heart.
- Blood tests - help the doctor to rule out the thyroid problems or other substances in the blood that may lead to atrial fibrillation.
- Chest X-ray - provides images of the structures in patient's chest, such as heart and lungs. This test can show fluid buildup in the lungs and signs of other AF complications.
- Transesophageal echocardiography (TEE) - is used to rule out the presence of clots in the atria.

Treatment
Treatment for atrial fibrillation depends on the frequency at which the symptoms occur, their severity, and whether the patient already has other heart problems. General treatment options include drugs, medical procedures, and lifestyle changes. The treatment of atrial fibrillation aims at:
- Preventing complications - caused by atrial fibrillation, such as blood clots, and thus lowering the risk of stroke
- Controlling current atrial fibrillation condition - including the restoration of normal heart rate and rhythm
- Treating the underlying disorders - that are causing or raising the risk of atrial fibrillation, such as hyperthyroidism.
Treatment with medicines includes the use of blood-thinning agents to prevent blood clots, medications controlling heart rate and heart rhythm. Doctors may use several methods to restore a normal heart rhythm, such as
- Electrical cardioversion - the external electric current is applied to restore the normal pattern of heart contraction.
- Catheter ablation - this is an invasive procedure which involves insertion of special flexible catheters into the heart. Local freezing or heating is used to destroy the abnormal tissues that cause arrhythmia.
- Open-heart surgical maze procedure - in the course of this surgery doctors make small incisions to create scar tissues in the heart. These tissues do not conduct electrical signals but direct them in a correct manner through a controlled path (maize).