Introduction
A pacemaker is a small device placed under your skin near to regulate your heartbeat. Normal aging of the heart as well as heart disease, heart attacks, and some medications can cause heartbeat abnormalities known as arrhythmias. These arrhythmias affect how well your heart pumps blood. Thus, an irregular heartbeat can potentially decrease the blood and oxygen supply to your tissues resulting in serious cardiovascular and respiratory conditions. However, a pacemaker can prevent or resolve all of this.
Who should get a Pacemaker?
Although primarily older patients receive pacemakers, it is not uncommon for younger people to undergo pacemaker surgery. After all, some genetic conditions that manifest shortly after birth cause arrhythmias. Either way, getting a pacemaker is a minor surgery with big results in spite of what may be causing your abnormal heartbeat.Pacemakers are ideal for both temporary and permanent conditions. So, if you are recovering from a heart attack or drug overdose, a pacemaker can help restore your heartbeat and then be removed. On the other hand, if you have a slow heartbeat or heart failure, a pacemaker can regulate your heartbeat for you for the rest of your life.

How Pacemakers work
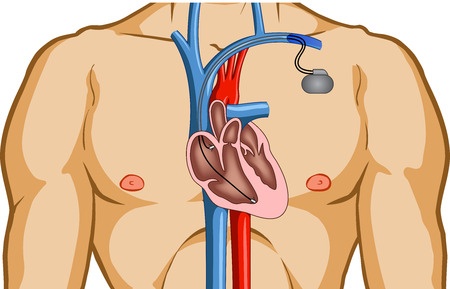
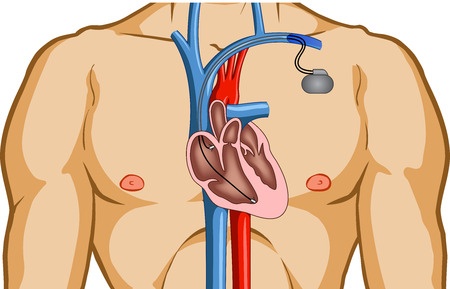
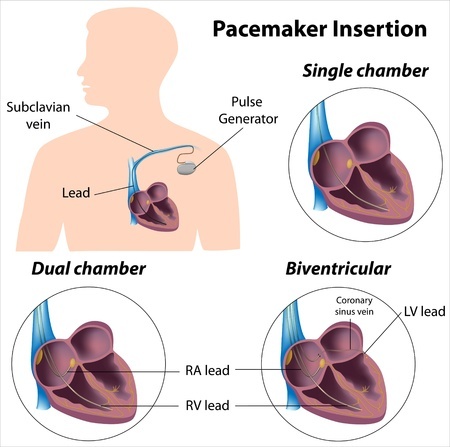
The heart is a four-chambered, muscular pump that functions via a coordinated, electrical system. Relatively perfectly timed electrical signals tell each chamber of the heart when to pump. But when that timing is disturbed, the heart pumps differently and an arrhythmia results.A pacemaker compensates for this inadequate timing. Pacemakers are made up of a pulse generator and leads or electrodes. The small, metal pulse generator contains a battery and electrical circuits that regulate the rate of electrical signals sent to your heart. The electrodes are all placed in one chamber or divided among the chambers of the heart to deliver the electrical signals and adjust the heart rate.
Pacemakers speed up your heart rate if your heartbeat is too slow. And they are designed to detect your body motion and breathing rate. So, pacemakers also increase your heart rate to meet your body’s need for blood and oxygen as you exercise or undergo other strenuous activities.
Planning your Pacemaker surgery
Your doctor must first perform some tests to find out what is causing your arrhythmia. These tests vary per person, but usually include a stress test, echocardiogram, electrocardiogram, and holter monitoring. After explaining how a pacemaker will improve your condition, your cardiologist may also recommend a specific type of pacemaker.- Single-chamber pacemakers - carry electrical signals from the pulse generator to the right lower chamber (right ventricle) of your heart.
- Dual-chamber pacemakers - carry electrical signals from the pulse generator to both chambers on the right side of the heart (right ventricle and right atrium).
- Biventricular pacemakers - stimulate both lower chambers of your heart (right and left ventricles) to overcome a damaged electrical system in the heart and reset its pumping mechanism.
Complications from pacemaker surgery are rare, but your cardiologist will inform you of some risks including allergic reactions, blood vessel or nerve damage, collapsed lung, infection, punctured heart muscle, and swelling around the site of the pulse generator.
How is Pacemaker surgery performed?
This surgery is usually performed with local anesthesia in a matter of a few hours. A nurse will shave your chest and write a number on the spot where your pacemaker will be inserted. He or she will also give you an intravenous antibiotic. Even though you will be given a sedative to relax, you will be awake during the procedure.In the more common endocardial method, your doctor will first make a small incision through your skin. Next, he or she will insert the pacemaker’s electrodes into a major vein under or near your collarbone and then guide them to your heart using X-ray images. Your doctor will then connect one end of the electrodes to the heart and the other end to the pulse generator. Finally, the pulse generator is placed under the skin in a pocket beneath your collarbone.
In the less common epicardial approach, reserved for children more so than adults, you will be put to sleep under general anesthesia. Then, the surgeon will connect one end of the electrodes to your heart and the other end to the pulse generator, which is placed in a pocket of skin in the abdomen.
After the surgery
Expect to stay in the hospital one day after your procedure. This allows time for your pacemaker to be programmed to fit the needs of your heart rate. Just one return visit to your doctor is necessary to check your pacemaker’s settings. Your doctor will advise you to avoid strenuous activity for about a month. And for any pain you experience, you may take acetaminophen or ibuprofen.After that, your doctor’s office can track your pacemaker activity wirelessly with radiofrequency signals or your cell phone. This transmission between your pacemaker and your doctor includes information about your heart rate, heart rhythm, pacemaker function, and its battery life. You can also send a transmission if you have a medical concern. This technology makes it possible for you visit your doctor less often. However, you will still need to go in for regular checkups.
Placing a cellphone over your pacemaker may confuse its detectors and cause you sudden fatigue. You should carry an ID card stating that you have a pacemaker to avoid potential problems during security checks that detect metal objects. If you work around power-generating equipment, inform your doctor of this and he or she can arrange to test this equipment to determine if it will affect your pacemaker. Yet, most devices like microwaves, televisions, and radios will not interfere with your pacemaker’s electrical system.