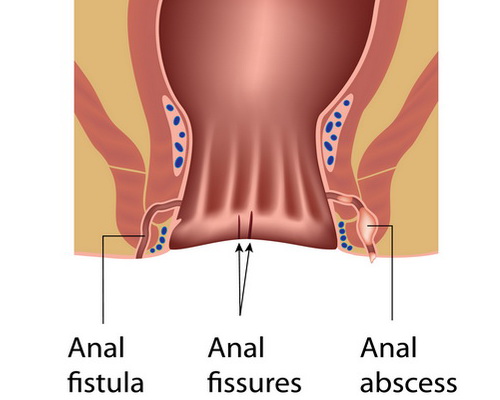
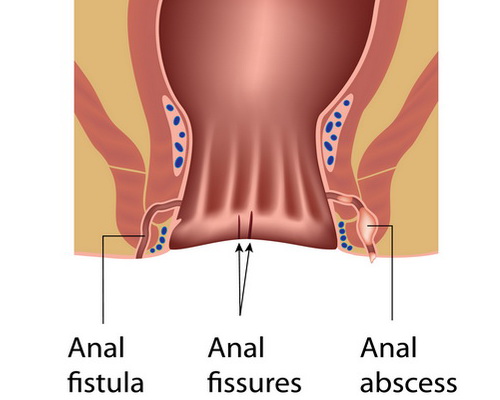
Overview
Anal fissures are cuts or tears in the lining of the anus that extend up to the anal canal. They form in the moist tissue that lines the anus, the mucosa, particularly in the posterior midline. This is thought to be explained by the unsupported nature and poor perfusion of the region, two factors that weakened it and make it prone to tears. The fissure can be superficial or go as deep as the muscle underlying the mucosa.Anal fissures can affect people of all ages and both men and women have equal chances of developing this condition.
Symptoms
Anal fissures can be associated with the following signs and symptoms:
- Pain, that can be severe, accompanying and following bowel movements
- Itching in the anal region
- Bright red blood on the stool or toilet paper after a bowel movement
- An identifiable tear around the anus
- A tiny lump on the skin around the anal fissure
- Yellowing discharge (pus) originating from the fissure
Risk factors
Anal fissures are caused by trauma inflicted to the anal canal. Patients whose sphincter muscles of the anus are too tense and patients with a decreased blood flow to the area have a higher risk of developing anal fissures. The latter is mainly the reason why anal fissures are so common in older people. Other risk factors include:- Infancy: anal fissures tend to develop in the first year of life, although the reason for that is not well known
- Constipation and diarrhea: both hard, dry bowel movements and loose stools increase the risk of tearing
- Childbirth
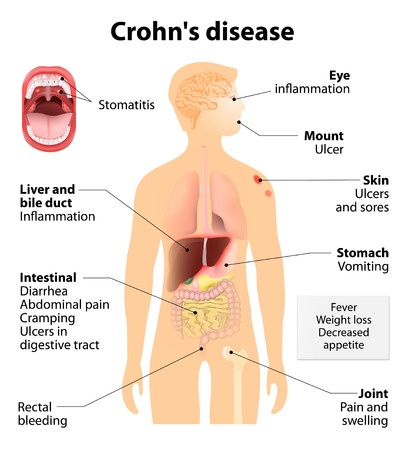
- Chron’s disease: this inflammatory disease causes the lining of the anal canal to be more fragile and thus more vulnerable to tearing
Diagnosis
Anal fissures can be diagnosed by a simple physical examination of the anal region. If no visible lesions are identified, the doctor may press the area gently and the resulting pain will confirm the existence of an anal fissure.Unless the anal fissure cannot be identified through mere observation, the digital rectal exam is not performed, since that is usually too painful for the patient. If the suspicion exists, but the identification is not possible, the doctor will use a small, lighted tube (anoscope) to take a look at the anal canal – this might be done under local anaesthesia.
Depending on the characteristics of the anal fissure, an underlying condition might be suspected and further testing will be ordered (a flexible sigmoidoscopy or a colonoscopy).
Treatment
Acute anal fissures heal in a few weeks by softening the stools. This can be accomplished by increasing the ingestion of fluids and foods rich in fiber. Soaking the region in warm water for a few minutes after bowel movements helps relieving the symptoms that follow. If these approaches are not enough to solve the problem, other options can be considered:- Externally applied medications - the application of medicines, such as nitroglycerin and calcium channel blockers, helps relaxing the sphincter muscles by reducing the blood flow to the region
- Botulinum toxin (Botox) - this substance paralyzes the muscles of the anal region, thus decreasing muscle spasms and improving symptoms
- Steroid creams - to decrease inflammation and relieve discomfort
- Surgery - if the patient has an anal fissure that does not resolve with the mentioned conservative methods (chronic anal fissures), the doctor might recommend surgery. This procedure involves removing part of the anal sphincter, which results in fewer spasms. About 95% of the patients that undergo this surgery have a great prognosis and the risk of faecal incontinence is minimal.