Overview
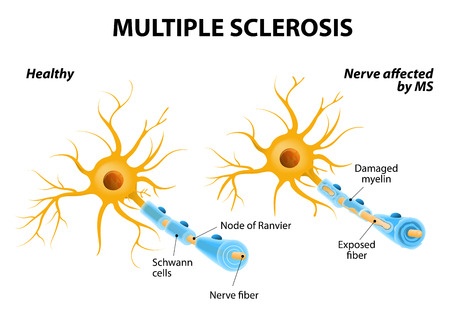
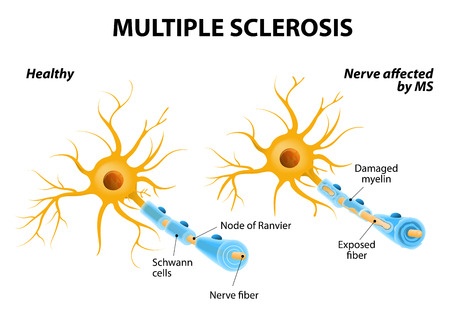
Multiple Sclerosis (MS) is an inflammatory disease, in which the patient’s immune system attacks the protective cover (myelin) of the nerve cells that make up the brain and the spinal cord. It belongs to the class of autoimmune disease. The consequent damages of such attacks are not reversible and interfere with the communications between the nerve cells. Symptoms differ among patients and depend on the level of deterioration and the nerves that are affected.The origin of the disease has not been clearly identified by the medical community, but it is thought to result from the interaction between a mixture of genetic and environmental factors. Multiple Sclerosis can arise in many forms, with the two major types being the relapsing forms (in which symptoms occur in isolated attacks) and the progressive forms (in which the condition tends to gradually worsen). Multiple Sclerosis is the most common cause of neurological disability in the early to middle-adulthood age ranges.
Symptoms
The symptoms of MS arise from the deficient communication between the nerve cells all over the patient’s body. Therefore, the range of symptoms is wide. Among others, the symptoms of MS include:
- Loss of sensitivity or changes in sensation (tingling, numbness, etc.)
- Various ocular problems, such as blurred vision and total or partial loss of central vision in one eye accompanied with pain during eye movements
- An electric-shock sensation that occurs when the patient bends the neck (Lhermitte’s sign)
- Muscle spasms, difficulties in coordination and balance
- Slurred speech
MS patients are very sensitive to the heat, and the exposure to temperatures higher than normal typically results in a worsening of symptoms, known as the Uhtoff’s phenomenon.
Risk factors
Predicting who is going to have MS and who is not is nearly impossible. However, several factors can put a person at risk for developing the disease:- Age - MS tends to appear between the ages of 20 and 40
- Gender - women are affected twice as more.
- Family history - if any direct family members have the disease (parents or siblings), the probability of developing the disease is 1-3%, compared to the risk of a 0.1% in the general population. However, studies in identical twins has suggested that genetic factors play only a small role in the development of the condition
- Infections - it is thought that certain infections are connected to the development of MS in some cases
- Ethnicity - MS is more common in northern European communities
- Geographic region - with a few exceptions, MS is more common in people who live far from the equator, in regions such as Europe, southern Canada, northern United States, New Zealand and South-Eastern Australia. Researchers found that if a person under the age of 15 moves to a different area of the globe, that person will acquire their new region’s typical MS risk. If the move happens after puberty, the person will have the same risk of developing MS as before.
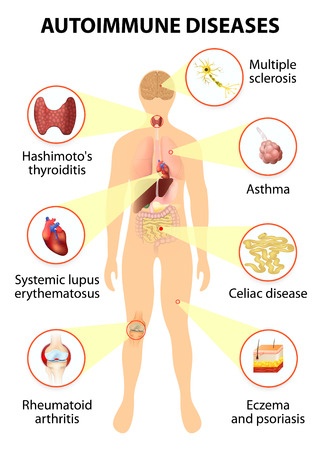
- Other autoimmune diseases - people who already have an autoimmune disorder, like type 1 diabetes or inflammatory bowel disease, are at a higher risk for developing the MS.
Diagnosis
Diagnosing the MS is not easy, primarily because of the diversity of symptoms and their varying intensity over time.Blood tests are done to rule out any infections or inflammations that might be causing the signs and symptoms. Analysis of cerebrospinal fluid is performed not only to rule out other conditions, but also to identify the eventual alterations associated with MS, such as an abnormal white cell count. MRI can reveal the presence of nerve cells without myelin, thus indicating the presence of the disease. Finally, the evoked potential tests can be done to evaluate the response of the brain to the electric stimuli applied to the legs and arms.
None of the above methods gives a definitive proof of the occurrence of MS. It is the mixture of evidences and the doctor’s clinical judgement and experience that allow for a diagnostics of MS.
Treatment
MS is not curable, so the primary goals of therapy are to manage attacks, to prevent new attacks and to slow down the progression of the disease.Intravenous corticosteroids are usually effective in the management of symptomatic attacks. Plasmapheresis might be an option for those not responding to the corticosteroids.
In order to avoid the disease progression, a number of drugs such as beta interferons, glatiramer acetate, fingolimod, dimethyl fumarate and others are available. The drugs are stopping the immune system from attacking the patient’s own body.
Symptoms of the disease can be improved by using certain types of pharmaceutical agents (such as muscle relaxants and medicines to reduce fatigue) and neurorehabilitation strategies (physical therapy, cognitive behavioural therapies, etc.).
Properly assessed patients have better chances of receiving the most suitable and effective therapy.